When To Switch To Advanced Chronic Wound Treatment Solutions
Wound care for a patient who isn't healing is one of the most frustrating aspects of clinical practice. That’s why advanced chronic wound treatment solutions are becoming the new standard for cases where conservative care stalls.
For many providers, the "standard of care" (SOC)—debridement, offloading, infection control, and moist dressings—works well for acute injuries. However, chronic wounds operate under a different set of biological rules.
When a wound remains open for more than 30 days, it enters a state of chaotic inflammation that standard dressings simply cannot fix. To understand why, we must look at the cellular mechanisms that cause traditional methods to fail and how modern therapies restart the healing process.
Why Traditional Wound Care Is Not Enough
Traditional wound care relies heavily on the body’s innate ability to heal. The goal of standard dressings is primarily protective. They cover the wound, manage exudate, and create a moist environment.
This passive approach assumes the patient’s cellular machinery is functioning correctly. In a healthy patient with an acute injury, this is a safe assumption.
However, in the Medicare demographic, often dealing with diabetes, venous insufficiency, or arterial disease, the cellular machinery is broken.
A standard alginate or foam dressing doesn’t actively correct the biological environment. It merely maintains the status quo. If the underlying tissue is stuck in a chronic inflammatory cycle, "maintaining" the wound stagnates instead of closing.
Stalled Healing at a Cellular Level
To understand why advanced chronic wound treatment solutions are necessary, we must look at what’s happening microscopically in a non-healing wound.
A chronic wound is biologically distinct from an acute wound. It’s characterized by a hostile microenvironment that actively destroys healing tissue.
The Protease Imbalance
Chronic wounds tend to have higher levels of Matrix Metalloproteinases (MMPs). While MMPs are necessary for clearing out damaged tissue in the early stages of healing, they become destructive when unregulated.
In a chronic wound, excess MMPs digest growth factors and new extracellular matrix (ECM) as fast as the body produces them.
Growth Factor Deficiency
In a healthy wound, growth factors act as the "general contractors," signaling cells to build new tissue.
In chronic wounds, these signals are either absent or degraded by proteases. Without these active signals, the repair process grinds to a halt.
Senescent Cells
Also called "zombie cells," these cells are metabolically active but have stopped dividing. They build up in chronic wounds and release pro-inflammatory cytokines. This fuels inflammation and prevents the transfer of healthy keratinocytes and fibroblasts.
Biofilm Formation
Bacteria in chronic wounds form a biofilm. It’s a protective slime layer that makes them resistant to systemic antibiotics and immune responses.
It’s rare for standard dressings to breach this barrier effectively.
When you apply a standard dressing to this environment, you’re essentially putting a bandage over a biological war zone. To change the equation, you need advanced therapies.
What Are Advanced Chronic Wound Treatment Solutions?
Advanced chronic wound treatment solutions refer to active therapies designed to interact with the wound bed to stimulate closure.
Unlike passive dressings, these products, specifically skin substitute grafts or amniotic membrane grafts, bring biological structure to the wound. These are made from human placental tissue (amniotic membrane). The placental membrane is rich in native extracellular matrix proteins, growth factors, and cytokines.
These solutions cover the wound and help shift the wound from a chronic, inflammatory state to an acute, proliferative state.
How These Solutions Improve Healing Outcomes
1. Scaffolding for Cell Migration
The extracellular matrix (ECM) in amniotic grafts serves as a scaffold. It gives the patient’s own cells a structure to climb across, bridging the gap that the body couldn’t close on its own.
2. Modulation of Inflammation
Advanced grafts contain natural properties that help soothe the excessive inflammatory response. By reducing inflammation, the wound can finally move into the remodeling phase.
3. Replenishment and Protection of Growth Factors
These grafts do more than just cover the wound; they’re biologically active. They deliver the native growth factors that chronic wounds lack, signaling the body to heal.
At the same time, the robust matrix protects these factors from being immediately destroyed by excessive MMPs.
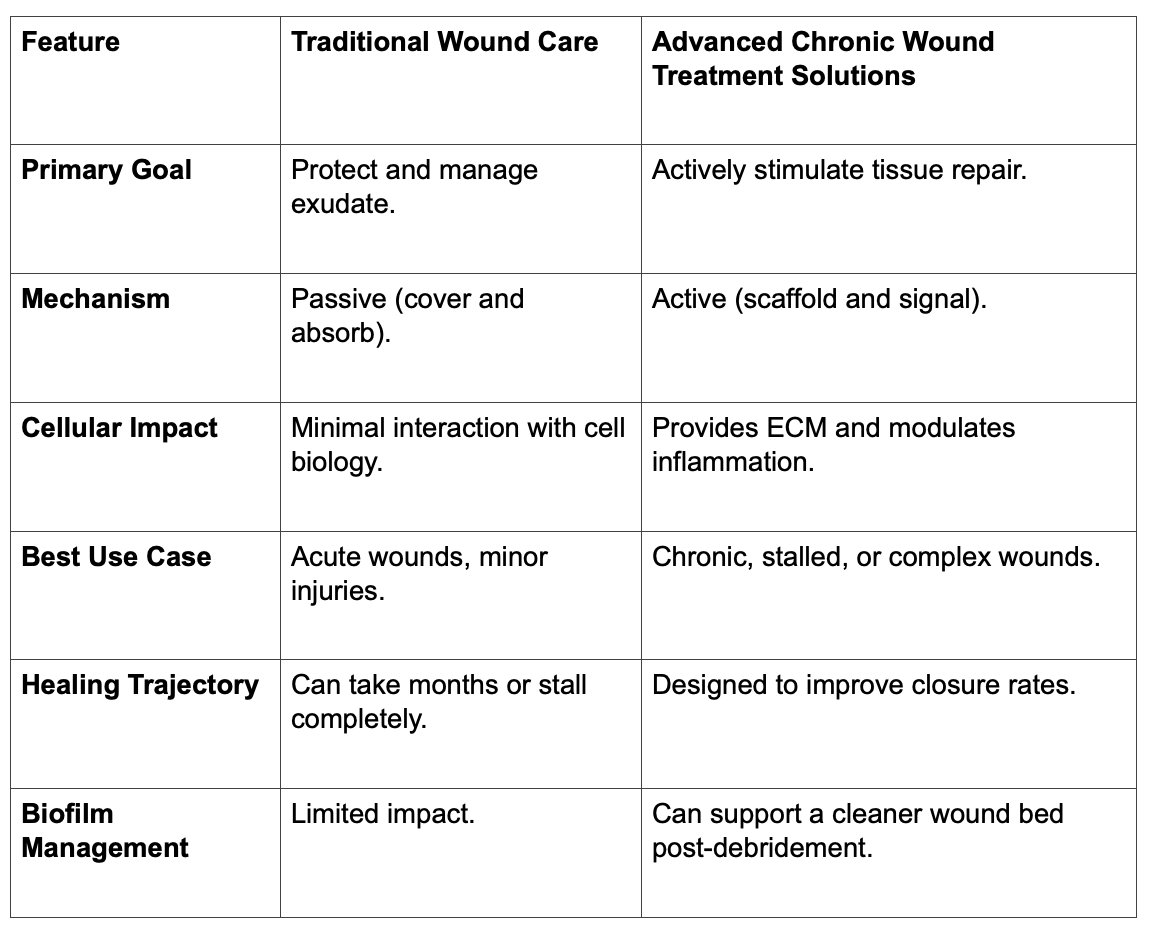
Comparison: Traditional vs. Advanced Wound Care
When to Implement Advanced Solutions
Knowing when to switch strategies is critical for both patient outcomes and practice efficiency.
You should consider advanced chronic wound treatment solutions when:
- A wound has not reduced in size by roughly 50% after four weeks of standard care.
- The wound has been present for more than 30 days (defining it as chronic).
- The patient has comorbidities like diabetes that impair natural healing.
- Visible granulation tissue is absent or pale, indicating stalled proliferation.
Waiting too long to escalate care increases the risk of infection, hospitalization, and even amputation. Early intervention with the right biologic can prevent these drastic outcomes.
Your Partner in Advanced Healing
Adopting advanced chronic wound treatment solutions is a clinical upgrade. But we know it presents administrative challenges. Many providers hesitate because of the paperwork, the fear of reimbursement clawbacks, or the complexity of ordering biologics.
This is where RenewMed steps in. We’re your White Glove Service partner, integrating the entire process into your practice.
We Handle the Heavy Lifting
- Insurance Verification. We manage the Insurance Verification Request (IVR) to ensure patient eligibility before you treat.
- Documentation Support. We provide guidance on the specific notes required to meet medical necessity standards.
- Reimbursement Confidence. Our team and specialized billing partners help you through the complexities of Medicare reimbursement.
- Streamlined Inventory. We manage logistics to ensure you have the correct graft sizes on hand, minimizing waste and optimizing costs.
- Dedicated Personal Consultant. You work with a single, dedicated expert who knows your practice. We don’t do the generic call center.
- Appeals Assistance. In the event of a denial, our partners assist with the appeals process to help protect the revenue you’ve earned.
We manage the product logistics, so you can focus on patient care.
Frequently Asked Questions (FAQs)
Are these advanced treatments covered by Medicare?
Yes, generally. Medicare covers specific advanced skin substitutes to treat chronic wounds, like Diabetic Foot Ulcers (DFUs) and Venous Leg Ulcers (VLUs). However, standard care must have failed, and the needed documentation requirements must have been met.
How do I know which graft size to order?
We assist with this. Grafts come in various sizes (measured in square centimeters). Minimizing waste is important for compliance and cost. Our team helps you match the product inventory to your patient needs.
Is the application process difficult?
No. Applying an amniotic graft is straightforward and can be done in the office setting. It typically involves:
- Debriding the wound.
- Placing the graft.
- Covering it with a non-adherent dressing.
How quickly will I see results?
While every patient is different, many clinicians report seeing positive changes in the wound bed within weeks of the first application.
Do I need to store these products in a special freezer?
It depends on the specific product line. Some are cryopreserved and require specific low-temperature storage. Others are dehydrated and shelf-stable at room temperature.
We help you choose the option that fits your facility’s capabilities.
Achieving Predictable Outcomes
Stalled wounds don’t have to remain that way. Advanced chronic wound treatment solutions provide the biological boost necessary to overcome the cellular limitations of chronic wounds.
Integrating these therapies into your practice protects your patients from prolonged suffering and sets your clinic apart as a leader in wound care.
Let’s discuss how we can support your practice.
Advance your clinical potential. Partnering for better outcomes, every single day.
Sources Used
- https://pubmed.ncbi.nlm.nih.gov/12766127/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC3623589/
- https://www.magonlinelibrary.com/doi/abs/10.12968/jowc.2017.26.1.20
- https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2020.00773/full
- https://onlinelibrary.wiley.com/doi/10.1111/iwj.12140
Disclaimer: This content is created for licensed healthcare professionals, offering educational insights into wound care. It is not intended as medical advice or to replace your own clinical judgment when treating patients. We're here to support you, but the final treatment decisions should always be based on your professional evaluation of each unique patient's needs.